- Lung Care Foundation
- 011 - 4225 2328
- lung@lcf.org.in
- Home
- About Us
- Our Initiatives
- Air Pollution
- Lung Basics
- Patient Support
- Get Involved
- Media
- Contact Us
Pulmonary Fibrosis
- Home
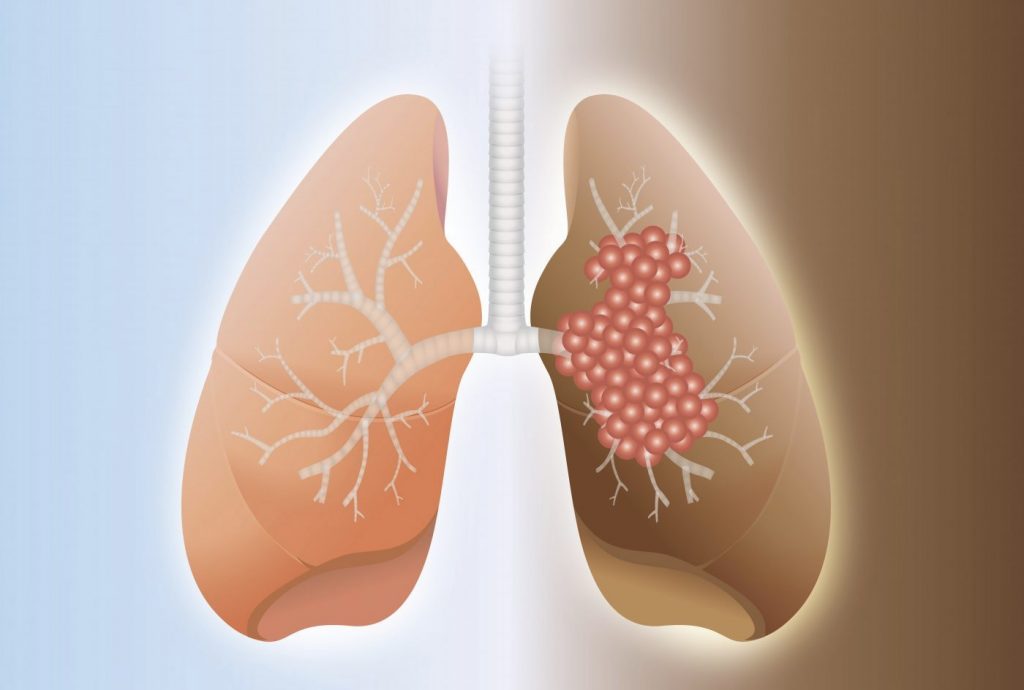
What is Pulmonary Fibrosis
Pulmonary fibrosis is a lung disease when the lung tissue becomes scarred, damaged and stiff making breathing difficult. This scar tissue can damage the lung over time making it difficult for oxygen to get into blood.
Due to the unavailability of oxygen, it may eventually lead to respiratory failure, heart failure or other complications.
Pulmonary fibrosis is one form of interstitial lung disease (ILD). There are more than 200 different ILDs, which include all the diseases that have inflammation and/or scarring in the lungs. When an interstitial lung disease does include scar tissue in the lung, we call it pulmonary fibrosis.
Causes
It is a challenging task to find out the exact cause as there are various causes due to which pulmonary fibrosis may occur but when the exact cause is unknown then it is known as Idiopathic Pulmonary Fibrosis (IPF).
The following table shows the causes of pulmonary fibrosis.
CAUSES OF PULMONARY FIBROSIS
Genetics
Combination of certain chemicals, smoking, and infections, along with genetics and immune system activity, play key roles in pulmonary fibrosis
Autoimmune Disease
Rheumatoid arthritis, Sjogren’s syndrome, Scleroderma
Occupational disease
Exposure to dusts, fibres, fumes, or vapours (asbestos, coal, silica, and others)
Idiopathic pulmonary fibrosis
Environmental disease
Drug-induced
Radiation-induced
Bacterial infection, viral infection
- Genetics: Combination of certain chemicals, smoking, and infections, along with genetics and immune system activity, play key roles in pulmonary fibrosis.
- Autoimmune disease: Rheumatoid arthritis, Sjogren’s syndrome, Scleroderma.
- Occupational disease: Exposure to dusts, fibres, fumes, or vapours (asbestos, coal, silica, and others).
- Idiopathic pulmonary fibrosis: Exact cause can’t be identified. It is the most common type of pulmonary fibrosis
- Environmental disease: Exposure to mould, animals, bird and animal dung.
- Drug-induced: Drugs used to treat cancer (chemotherapy), abnormal heart rhythms (such as amiodarone), inflammatory conditions (such as methotrexate), and an antibiotic used to treat urinary tract infections (nitrofurantoin).
- Radiation-induced: Prior or current radiation therapy for lung or breast.
- Infection: Bacterial infection, viral infection.
Risk Factors
Certain factors that make you more susceptible to pulmonary fibrosis include:
- Age: Pulmonary fibrosis can be more likely to be affected among middle and old age groups i.e. 40-70 years but it has been also diagnosed in children and infants.
- Sex: Affect more likely men than women
- Smoking: Those with the history of smoking or current smokers can develop pulmonary fibrosis.
- Certain occupations: Working in an occupation associated with mining, farming or construction or if you’re exposed to pollutants can increase the risk of harm to lungs.
- Medicines and radiation treatment: If one has undergone cancer treatment such as radiation treatments to your chest or using certain chemotherapy drugs or medications associated with the disease.
- Genetic factors: Having a family history of pulmonary fibrosis can increase the chances for the same.
- People with autoimmune disorder
Symptoms
The first symptom of pulmonary fibrosis is shortness of breath.
As the lungs develop more scar tissue, symptoms worsen and patients may become breathless while taking part in everyday activities, such as showering, getting dressed, speaking on the phone, or even eating.
The symptoms of pulmonary fibrosis are:
- Shortness of breath
- Clubbing - due to lack of oxygen in blood there is a thickening of the flesh under the fingernails, causing the nails to curve downward.
- Continuous, dry cough
- Fatigue
- Weight loss
- Stiff joints and muscles
Diagnosis
First of all, your doctor will ask you about your medical history and symptoms, and then examine you looking for causes of breathlessness.
During the physical examination, the doctor with the help of a stethoscope will look to hear for crackle sound to your lungs for those suffering from pulmonary fibrosis.
If any suspicion further test will be conducted such as:
1. Chest X-ray
It may show a scar tissue of the lungs. Sometimes the chest X-ray may be normal, and further tests may be required to explain your shortness of breath.
2. CT scan of lungs
Some of the diagnosis for pulmonary fibrosis can be done easily with the help of a CT scan which reveals a honeycomb type of appearance.
3. Lung function tests
With the help of spirometry, the lung volume capacity is measured where one needs to forcefully take in the air and blow out with the same force.
4. Blood tests
To look for any cases of infection, anaemia or any autoimmune diseases.
5. Arterial blood gas test
To assess the oxygen level in your blood this test is done by taking a sample of your blood from an artery in your wrist.
6. Tissue Biopsy
To get more information your doctor may need to remove some tissues or cells for testing.
The different procedures are: Bronchoscopy and video-assisted thoracoscopy (VATS)
-
Bronchoscopy
Under local anaesthetic, bronchoscope which is a small, flexible narrow tube inserted through your mouth or nose into your lungs with a camera on the end so to see the inside of lungs. Small piece of lung tissue is removed for further testing -
Video-assisted thoracoscopy (VATS)
This is done under general anaesthesia, with the removal of a large piece of lung tissue using surgical instruments and a small camera that is inserted through two or three small incisions between your ribs.
Treatment
Medications and therapies can help to ease symptoms and improve quality of life though the lung scarring occurred can’t be reversed.
The treatments below are used for managing pulmonary fibrosis:
Medication
To suppress your immune system.
Supplemental oxygen
A therapy in which your body is provided with extra oxygen to support the important functions of the body in case of heart or lung disease.
Lung transplant
A lung transplant may be the only option left for people with pulmonary fibrosis. If your doctor thinks you are suitable for it then you’ll be referred to a transplant unit for further assessment.
Pulmonary rehabilitation
This can help in improving your daily functioning which focuses on:
- Physical exercise
- Education and support to help learn how to breathe more easily
- Breathing technique
- Proper nutrition counselling
Prevention
Prevention is better than cure; you can take care of yourself by:
- Avoiding smoking and also second-hand smoke
- Having a proper balanced diet
- Adequate rest is a must
- Avoid stress
- Do proper and regular exercise as advised by your doctor’s
Questions for your Doctor
- What must be the reason for me to get pulmonary fibrosis?
- I heard that in this problem our lungs don't get reversed back, then will I lead an abnormal life?
- Will anything help me to breathe better again?
- If I have IPF will my children also suffer?
- Do I need to get a lung transplant?
Frequently Asked Questions (FAQs)
PF belongs to a group of lung disorders called interstitial lung diseases (ILD). It is a progressive disease marked by fibrosis, or scarring of lung tissue, that makes breathing difficult and affects lung function.
The diagnosis of PF requires multiple tests, including chest X-rays, lung function tests, and pulse oximetry. A biopsy of the lungs may be needed to rule out other lung diseases.
The progression of PF can be categorised into stages based on the results of forced vital capacity (FVC) tests, determined by spirometry. The staging is as follows:
FVC greater than 75% — mild disease
FVC between 50 and 75% — moderate disease
FVC between 25 and 49% — severe disease
FVC lower than 25% — very severe disease
No. PF is not contagious and does not spread from person to person.
All Rights Reserved By LCF.ORG.IN | Privacy Policy | Terms and Conditions
Powered by: www.chillitrends.com
- Home
- About Us
- Our Initiatives
- Air Pollution
- Lung Basics
- Patient Support
- Get Involved
- Media
- Contact Us