- Lung Care Foundation
- 011 - 4225 2328
- lung@lcf.org.in
- Home
- About Us
- Our Initiatives
- Air Pollution
- Lung Basics
- Patient Support
- Get Involved
- Media
- Contact Us
Lung Cancer
- Home
What is Lung Cancer?
Lung cancer is a type of cancer that starts in the lungs. It is also called primary lung cancer. If it starts in another part of your body and spreads to affect your lung, it’s called secondary lung cancer.
There are two major types of primary lung cancer. Each type of lung cancer grows and spreads in different ways and maybe treated differently.
Non-small cell lung cancer
This is the most common type of lung cancer. It usually spreads more slowly than other lung cancers.
There are three major types of non-small cell lung cancer:
- Squamous cell carcinoma
- Adenocarcinoma
- Large cell carcinoma
Out of these, Adenocarcinoma is the particular type which can occur in people who never smoked.
Small cell lung cancer
This is a less common type of lung cancer and it spreads faster than non-small-cell lung cancer. Small cell lung cancer is named after the size of cancer cells, which can only be seen under a microscope.
Causes
Anyone can get lung cancer. Lung cancer happens when cells in the lung mutate or change. Various factors can cause this mutation (a permanent change in the DNA sequence of a gene) to happen. Most often, this change in lung cells happens when people breathe in dangerous, toxic substances.
1. Smoking
Around 90% of cases of smokers has a higher risk of developing lung cancer though it can also occur to non-smokers.
Your risk of getting lung cancer increases with the number of cigarettes you’ve smoked and the number of years you’ve been a smoker. If you stop smoking, the risk gets lower over time.
2. Non-Smokers
Some people who have lung cancer have never smoked a day in their lives. The risk factors for non-smoker are:
-
Second-hand smoke – People who breathe second-hand smoke i.e. inhalation of tobacco smoke from the surroundings have almost double the risk of getting lung cancer than people who stay away from smoke.
“Non-smokers who live or work in smoky air can get lung cancer from second-hand smoke”
-
Radon – Radon is a colourless, odourless, and naturally occurring gas found in the soil that can enter through cracks in the foundation or insulation of the building, or drains, or walls. Radon can get trapped in basements and other places that don’t have a lot of airflows (fresh air). A higher concentration of radon is indoor than outdoor.
One can’t taste, see or smell it. People who have high exposure to radon are at higher risk of lung cancer.
- Asbestos – Asbestos is a heat-resistant mineral and consists of six naturally occurring silicate minerals, found in some workplaces and homes. It has been used in brake pads, insulation, siding, and many other products. People who have high exposure to asbestos are at higher risk of lung cancer.
- Air pollution – It is been the most leading cause of developing lung cancer. The increase in pollution level from vehicles, factories have led to an increase in lung cancer cases among the non-smokers.
- Other toxic products – Uranium, arsenic, some petroleum products may also increase the risk of developing lung cancer.
Symptoms
When the mutated cells increase in number it leads to the formation of a lump called tumour. Symptoms depend upon the severity of the tumour until it becomes quite large. This means it might only be discovered when you have an X-ray or scan for a different reason.
Most lung cancer patients don’t have any symptoms. As your condition progresses, you may begin to experience symptoms, such as:
- Cough
- Feeling out of breath
- Chest pain
- Feeling tired
- Appetite and weight loss
- Hoarse voice
- Blood in mucus or phlegm
- Swelling of lymph nodes
People with these symptoms could have lung cancer, or it could be something else. If you have these symptoms, you should see your doctor.
Diagnosis
Your diagnosis depends upon the medical history, examination of your body, and by further tests.
1. Medical History
Your doctor may ask:
- Any past or present medical problem?
- Smoking history- if you are a smoker how many cigarettes per day and for how long? If no, were you exposed to second-hand smoke?
- Where you lived and worked and what kind of work have you done?
- What is your family history of cancer?
- What symptoms have you noticed?
In case the examination suggests cancer, then your physician might advise for further tests.
2. Imaging Tests
Your doctor might order imaging tests that may help to find lung cancer. The test may be advised before or after the diagnosis of cancer.
Imaging tests make pictures of the inside of your body which help the doctors to know if:
- There are signs of lung cancer
- Cancer has spread to other parts of the body
- Treatment is having a positive effect or not
- Cancer has come back even after treatment.
These tests include:
- Chest X-ray
- Computed tomography (CT) scan
- Positron emission tomography (PET) scan
- Magnetic resonance imaging (MRI) scan
- Bone scan
3. Test done through procedures
To see if there is something suspicious, the doctor studies the tissue or fluid from or around the lung. Many different procedures allow doctors to remove cells from the body and look at them under a microscope to determine if they are cancer.
These tests include:
- Bronchoscopy – It is examining your airways and visualizing the tumour in them. For a bronchoscopy the person needs to be sedated (under general anaesthesia). Then, the doctor slides a thin, flexible tube (a bronchoscope) through your mouth or nose and into your lungs. Bronchoscopy can be done on the same day.
- Sputum cytology – The doctor collects your sputum (the phlegm you cough up) and tests it for cancerous cells.
- Fine needle aspiration (FNA) – Local anaesthesia is given and a thin needle is slid into your chest. The needle collects a small piece of the tumour, which doctors examine under a microscope.
- Endobronchial Ultrasound (EBUS) – Bronchoscope (a thin, lighted, flexible tube) is fitted with an ultrasound device (a device that uses sound waves to take pictures of the inside of your body) at its tip. It is passed down into the windpipe to look at nearby lymph nodes and other structures in the chest. This is done with numbing medicine (local anaesthesia) and light sedation.
- Endoscopic Oesophageal Ultrasound (EUS) – This test is much like an endobronchial ultrasound, except that an endoscope (a lighted, flexible tube) is used. It is passed down the throat and into the oesophagus.
- Mediastinoscopy and mediastinotomy – This procedure is done by looking closely at the area between the lungs and getting a sample from it. The procedure is conducted under general anaesthesia (in a deep sleep). The doctor makes a small cut in your neck and inserts a thin tube. The tube collects fluid samples and biopsies (pieces of tissue) from the lymph nodes near your throat and lungs. If through mediastinoscopy, lymph nodes cannot be removed then through mediastinotomy biopsy sample can be directly removed. This test helps your doctor know if cancer has spread to any of your lymph nodes.
- Thoracentesis – This test is done to check whether fluid around the lungs is caused by cancer or by some other medical problem. A needle is placed between the ribs to drain the fluid and is further checked for cancer cells.
- Thoracoscopy or video-assisted thoracic surgery (VATS) – A small cut is made in the chest. The surgeon then uses a thin, lighted tube connected to a video camera and screen to look at the space between the lungs and the chest wall. The surgeon can see small tumours on the lung or lining of the chest wall and can take out pieces of tissue to be looked at under the microscope. This procedure is only done if other procedures like needle biopsies fail to extract samples for diagnosis.
4. Lung Cancer Screening: Test For Healthy Individuals
Screening is looking for cancer before you have any symptoms, which can help find cancer at an early stage when it may be easier to treat. It is done annually and for those who have a risk of cancer.
Data show that screening for lung cancer with low-dose computed tomography (LDCT) reduces the risk of dying from lung cancer in the high-risk population studied. Other screening tests such as chest X-rays and sputum cytology are not effective and are not recommended for screening.
If you meet the following criteria, you are considered to be at “high risk” for developing lung cancer and screening is recommended:
- 55-80 years of age
- Heavy smokers: Smoked around 30 pack-year history of smoking (this means 1 pack a day for 30 years, 2 packs a day for 15 years, etc.). Current smoker, or have quit within the last 15 years
5. Lung Cancer Staging
Staging means finding out how much cancer has spread in the body. The treatment plan and the general outlook for your recovery depend upon staging by evaluating the size and shape of tumour.
Three factors are used to determine the lung cancer stage (sometimes referred to as the TNM classification system).
- T – Tumour size and location
- N – Regional lymph node involvement. Lymph nodes are small ball-shaped immune system organs distributed throughout the body. It is important to know whether the lung cancer has spread to the lymph nodes around the lung.
- M – Metastasis status. Metastasis status refers to which organs cancer has spread.
- Limited SCLC: where the cancer confined to the area of lungs
- Extensive SLSC: where the cancer has spread to other parts of the body
Treatment
Different treatments work for different types of lung cancer. To decide on treatment for a particular patient, doctors look at:Pump or Puffer
- Type of cancer
- Patient’s age and overall health
- Stage of lung cancer
After looking at those factors, doctors may recommend one or more of these treatments.
Surgery
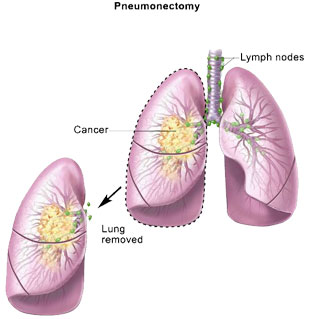
Pneumonectomy Doctors remove one entire lung (people can breathe using the remaining lung).
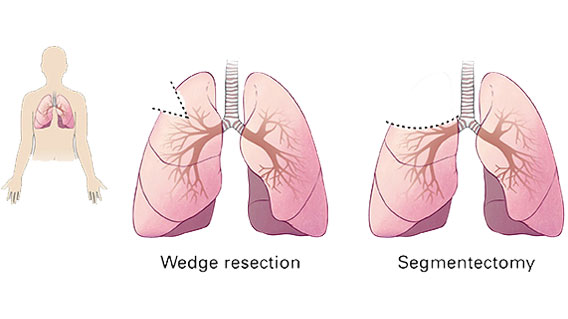
Segmentectomy or wedge resection: Doctors remove a section of the lung (a lobe).
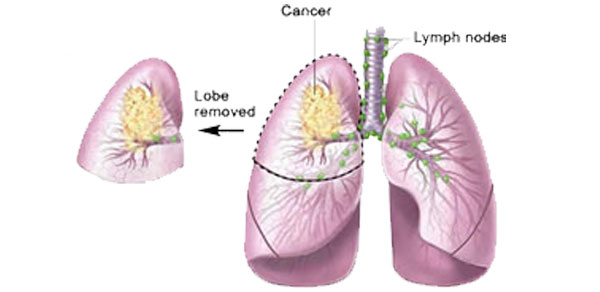
Lobectomy: Doctors remove a part of a lobe.
Laser surgery: A high-energy beam of light destroys the cancer cells in a tumour.
Chemotherapy
Chemotherapy is a therapy that fights against the cancer. Some kinds of chemotherapy come in pills. Other kinds are delivered into your bloodstream by intravenous drip (IV), where a machine slowly drips medicine into tubes that go into your veins. Some chemotherapy is given by injection (a shot).
It is often used after surgery to kill the remaining cancer cells. Chemotherapy is used before surgery for easy removal of the cells by shrinking them.
Radiation Therapy
Radiation therapy uses high-energy radiation to kill cancer cells by aiming beams of radiation from different angles. The radiation can be delivered by a machine that directs the high-energy rays towards cancer, or by a small radioactive pellet that gets implanted in or near the tumour.
Management
-
✔ Pulmonary rehabilitation –
Fighting against illness and diseases leads to a negative impact on our body and affects our daily activities and lifestyle, so pulmonary rehabilitation with the help of exercise and making one aware by educating them can help in managing their health and lifestyle.
-
✔ Smoking cessation –
The major cause of lung cancer is smoking, so to prevent the recurrence or to stabilize your condition better to quit smoking.
-
✔ Eat fresh fruits and vegetables –
A proper and balanced diet is a must for those who had or have cancer. Eating healthy food can help you in gaining strength.
Questions for your Doctor
- What kind of cancer do I have?
- Why did it occur?
- Is my cancer spreading faster? Which stage of cancer is it?
- Do I need to get chemotherapy and radiotherapy started?
- Should I get the second opinion?
- Will my whole of the lung be removed?
- Do I need to get a lung transplant?
- Will I be able to perform my daily routine and physical activity after surgery?
- What will be the major side effects of my cancer treatment?
Frequently Asked Questions (FAQs)
This information was provided by the Gynaecologic Cancer Foundation.
Who gets lung cancer?
Doctors estimate that over 90 percent of lung cancer cases are related to smoking. However, a small percentage of people who get lung cancer do not have a history of smoking or being around second-hand smoke. So, not all smokers get lung cancer and not all lung cancer patients were smokers.
There is really no way to know for sure if a woman is going to get lung cancer. What can a woman do about risk factors? Since it is known that smoking tobacco causes most cases of lung cancer, a woman who smokes would benefit from quitting as soon as possible, even after being diagnosed with lung cancer. When a woman quits smoking, her risk of getting the disease declines over time. Non-smokers can benefit from never starting and from staying away from those who do smoke.
Smoking is known as a controllable risk factor. Quitting greatly reduces a woman’s chances of getting lung cancer. In fact, quitting smoking can greatly reduce a woman’s risk of many other cancers as well. These include cancers of the bladder, pancreas, larynx, mouth, oesophagus, pharynx, and kidney. There are many ways to quit smoking. Women who would like to quit smoking should talk to their doctor about creating a plan to quit. Should everyone get a second opinion? Many people with cancer get a second opinion from another doctor. There are many reasons to get a second opinion, including if the person is not comfortable with the treatment decision, if the type of cancer is rare, if there are different ways to treat the cancer, if there may be clinical trials available for this type of cancer; or if the person is not being treated by a lung cancer expert. How can someone get a second opinion? There are many ways to get a second opinion:
- The person’s primary doctor may be able to recommend a specialist such as a surgeon, medical oncologist, radiation oncologist, or plastic surgeon. Sometimes these doctors work together at cancer centres or programs.
- Patients can get names of doctors from their local medical society, a nearby hospital, a medical school, or local cancer advocacy groups, as well as from other people who have had that type of cancer.
All Rights Reserved By LCF.ORG.IN | Privacy Policy | Terms and Conditions
Powered by: www.chillitrends.com
- Home
- About Us
- Our Initiatives
- Air Pollution
- Lung Basics
- Patient Support
- Get Involved
- Media
- Contact Us
